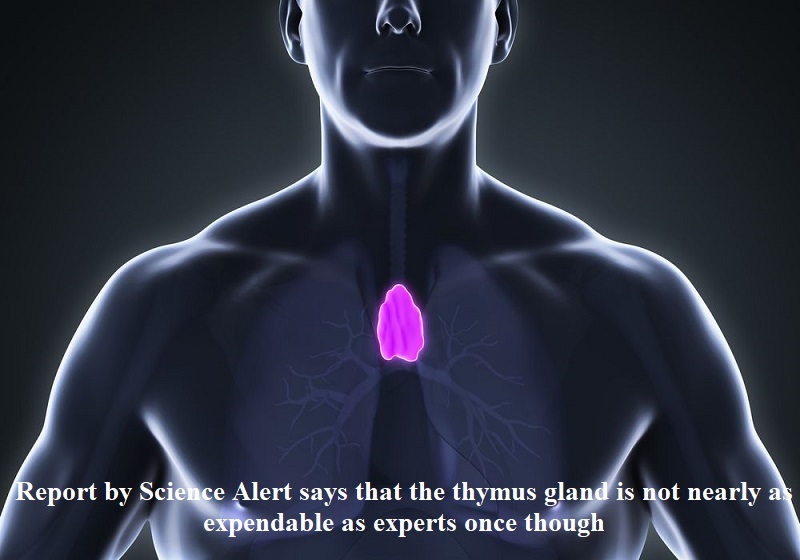
Previously regarded as functionally insignificant in adulthood, the small fatty gland positioned behind the sternum could possess notable advantages and even contribute to the battle against cancer. Drawing upon a recent retrospective study, a Science Alert report published on Monday (August 14) challenges the conventional belief that the thymus gland is nonessential. Researchers in the United States have discovered through their investigation that individuals who undergo thymus removal are exposed to an elevated risk of mortality from various causes in their later years. Additionally, this group faces an augmented susceptibility to cancer development.
The findings of the study, presented in the New England Journal of Medicine, strongly advocate for prioritizing the retention of the thymus gland whenever feasible. The researchers contend that safeguarding the thymus “should be a clinical priority.” Furthermore, they postulate that the adult thymus likely plays a pivotal role in upholding immune competence and overall well-being.
This disclosure upends the prevailing assumption that the thymus, frequently dismissed as irrelevant beyond childhood, serves minimal function in adulthood. Instead, the research underscores the gland’s crucial contribution to health, encompassing the intricate realm of immunity and potentially curtailing the onset of cancer.
During childhood, the thymus plays a pivotal role in immune system development. When the gland is removed at a young age, patients exhibit a long-term reduction in T-cells, a subset of White Blood Cells (WBCs) that combat pathogens and ailments.
However, once an individual reaches puberty, the thymus undergoes atrophy and produces significantly fewer T-cells for the body. The thymus can be excised, a procedure frequently carried out during cardiothoracic surgeries. Patients afflicted with thymus cancer or chronic autoimmune conditions necessitate thymectomy, a surgical removal of the thymus.
The study methodically assessed the risk of death, cancer, and autoimmune disease among adult patients who underwent thymectomy, comparing them to demographically matched controls who underwent similar cardiothoracic surgery without thymectomy. The investigation encompassed 1420 patients who had undergone thymectomy and 6021 controls, with a primary cohort of 1146 patients and matched controls.
Ultimately, the study revealed that five years following surgery, the thymectomy group exhibited higher all-cause mortality and cancer risk compared to the control group. The disparity in autoimmune disease risk was more pronounced when patients with preoperative infection, cancer, or autoimmune disease were excluded from the analysis.

Post Your Comments